If you want to do right by the planet, the general advice is to eat an abundance of fruit and vegetables, as well as whole grains and nuts, and to consume less meat, dairy and processed foods. Add some high-fibre fare, fermented food and fish a few times a week, and you could be eating your way to better mental health, too.
Those are the recommendations from nutritional psychiatry research. The field is built around growing evidence from population studies and clinical trials in the past decade suggesting that dietary improvements might not only improve mood but also treat common and severe mental illnesses. Traditional diets consumed by people in places such as the Mediterranean, Norway and Japan are associated with a lower risk of depression — one of the most common mood disorders — and, to a lesser extent, anxiety. A change in diet can alleviate symptoms of depression, even among people with severe forms of the condition.
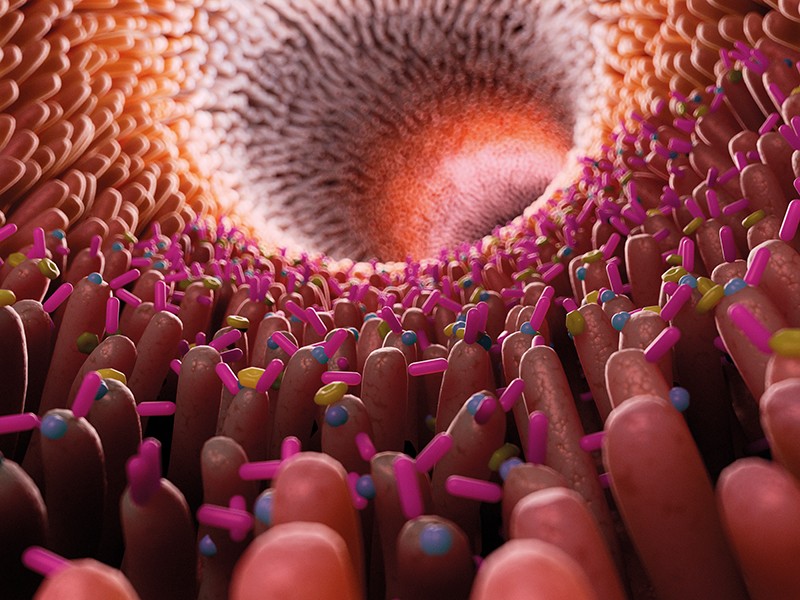
Researchers have also been investigating how the trillions of microorganisms in the human gut communicate with the brain to influence the processes that take place there. Imbalances in the gut microbiome have been linked to a range of neurological disorders, including Alzheimer’s disease, autism spectrum disorder, multiple sclerosis, Parkinson’s disease and Huntington’s disease.
Brain function, mood and mental health seem to be intricately linked to what people eat through the gut–brain axis, which is modulated by the gut microbiome.
That there is a connection between the food people eat and the brain is “something that ancient wisdom has been telling us for a long time”, says Amy Loughman, a gut-microbiome researcher at Deakin University’s Food and Mood Centre in Geelong, Australia. “But it’s really exciting that science is beginning to prove how and why.”
The gut microbiome is proving to be extremely complex and sensitive. Changes in diet can alter its composition in days. But the data from human trials on dietary interventions designed to shift gut microbiota to improve mental health are mixed, according to one meta-analysis1. Some studies of probiotics — live microbes that, when introduced in adequate quantities, confer health benefits on the host — have had compelling results, such as reduced symptoms of depression in women who have recently given birth. But others have shown no more effect than a placebo. Comparisons are difficult owing to the varying doses and strains of bacteria used in trials. Similarly, although promising, the evidence from human trials testing specific prebiotic foods — those that are rich in high-starch dietary fibres that stimulate beneficial bacterial colonies in the gut — is insufficient to draw clear conclusions.
At the Food and Mood Centre, researchers focus on the entire diet, rather than individual ingredients or certain strains of bacteria delivered in probiotic supplements. “There are no superfoods that are going to guarantee positive mental health,” says Loughman. “It’s both simpler and more complex than that.”
To support mental and brain health, high-fibre foods such as fruit, vegetables and whole grains are recommended, Loughman says. In these foods, the fibre and starches that are resistant to digestion in the small intestine promote the growth of beneficial bacteria, which guard against inflammation by protecting the gut wall. The bacteria also produce the short-chain fatty acids that are thought to have a key role in crosstalk between the gut and the brain. Chemicals such as polyphenols in plant-based foods and omega-3 fatty acids in fish have reported mental-health benefits, too. To get them all, people need to eat a well-rounded diet.
On the question of what mix of microbes makes for a healthy microbiome, diversity is thought to be important. People with a greater variety of bacteria in their gut seem to be healthier. A Western diet of processed foods that is high in fat and sugar and low in dietary fibre and micronutrients seems to be detrimental to both the gut and the mind, reducing the diversity of the gut microbiome, increasing inflammation and elevating the risk of depression.
The long-running SUN (Seguimiento University of Navarra) cohort study has been recruiting university graduates in Spain since 2000 to analyse associations between dietary patterns and health, including depression. One of its findings is that the more ultra-processed foods (usually, energy-dense foods that are significantly altered from their original state) you eat, the greater your risk of depression2. Over the past decade, observational studies of this kind have consistently shown that well-rounded diets that are low in ultra-processed foods confer some protection against depression. But public-health researcher Almudena Sánchez Villegas at the University of Las Palmas of Gran Canaria, Spain, says more randomized controlled trials testing specific dietary interventions are needed. This will allow researchers to refine the International Society for Nutritional Psychiatry’s existing dietary guidelines3 for preventing depression, of which Sánchez Villegas is a co-author. Because individual responses to food seem to be mediated by a person’s gut microbiome, researchers will need larger trials to work out who is likely to benefit from dietary interventions before these can be prescribed in the clinic. Until then, the public-health message is simple: everyone stands to benefit from a balanced diet with plenty of fruit, vegetables and fibre, and few processed foods. “That’s universally good for people,” says Loughman.



/assets/images/provider/photos/2672875.jpg)

More Stories
Censorship and Health Propaganda: The Hidden Dangers
Can You Trust Government Health Agencies Anymore?
Eating Disorders Information Every Family Should Read